According to a recent estimate, the so-called Spanish influenza pandemic of 1918 was as lethal as WWI (17 million killed) and WWII (60 million killed) combined, killing between 50 and 100 million.
One theory is that it began when the cook at a soldier's camp at Funston, Kansas, became sick in the morning of 4th March, 1918. By the evening, about 100 people were sick. Funston sent soldiers to other camps in the US and to France, at the front. The flu soon spread to other countries.
Spain's population was about 20 million, of which 8 million contracted the flu and 300,000 died. Thus the mortality rate in Spain was a little under 4%. It is called the Spanish flu because Spain, being neutral during WWI, did not impose censorship on news of the epidemic. Other countries were worried about combat morale and so imposed censorship. Because of this, it erroneously seemed that Spain was hardest hit, hence the unjustified name.
In the US, about 28% of the population of 105 million became infected, and 500,000 to 675,000 died (about 0.5% of the population). In the Fiji islands, it killed 14 percent of the entire population in 16 days. Worst affected was Western Samoa. 90% of the population was infected; 30% of adult men, 22% of adult women, and 10% of children died. By contrast, Governor John Martin Poyer prevented the flu from reaching neighboring American Samoa by imposing a blockade, so that there were no infections.
The pandemic infected 500 million, one quarter of the world's population. It killed between 1 and 6 percent of the total population, suggesting an estimate of 20 million killed, which is probably a severe under-estimate. Only some extremely remote parts, such as Antarctica and the Amazon were spared. Most people died during a period of 13 weeks in 1918.
The epidemic came on in three distinct waves, each lasting two or three months. The second wave was the worst. This was because the virus had mutated to a much more deadly form. The third wave finished in 1920. A study has shown that human behavioural responses had the most significant effects on the timing of the three waves. After the lethal second wave struck in late 1918, new cases dropped abruptly - almost to nothing after the peak in the second wave.
Even if isolation only slowed the virus, it had some value. One of the more interesting epidemiologic findings in 1918 was that the later in the second wave someone got sick, the less likely they were to die, and the more mild the illness was likely to be. Australia, which was not hit by the second wave until 1919, had the lowest death rate of any developed country. It is probable that the 1918 virus mutated extremely rapidly to a less lethal strain. This is a common occurrence with influenza viruses: there is a tendency for pathogenic viruses to become less lethal with time, as the hosts of more dangerous strains tend to die out.
The increased severity of the second wave has been attributed to the circumstances of the First World War. In civilian life, natural selection favours a mild strain. Those who get very ill stay home, and those mildly ill continue with their lives, preferentially spreading the mild strain. In the trenches, natural selection was reversed. Soldiers with a mild strain stayed where they were, while the severely ill were sent on crowded trains to crowded field hospitals, spreading the deadlier virus.
The war also contributed because of over-crowding, the weakness of the soldiers and the movement of troops. On 11.11.1918, the day of the armistice, the numerous celebrations provoked a virulent explosion of the flu.
Focusing on the shortest term, local officials almost universally told half-truths or outright lies to avoid damaging morale and the war effort. When influenza first appeared, officials routinely insisted at first that it was only ordinary influenza, not the Spanish flu. As the epidemic exploded, officials almost daily assured the public that the worst was over. Chicago's public health commissioner said he'd do "nothing to interfere with the morale of the community... It is our duty to keep the people from fear. Worry kills more people than the epidemic". In Philadelphia, when the public health commissioner closed all schools, houses of worship, theatres, and other public gathering places, one newspaper went so far as to say that this order was "not a public health measure" and reiterated that "there is no cause for panic or alarm."
But as people heard these reassurances, they could see neighbours, friends, and spouses dying horrible deaths. This horrific disconnect between reassurances and reality destroyed the credibility of those in authority. People felt they had no one to turn to, no one to rely on, no one to trust. One lesson is clear from this experience: In handling any crisis, it is absolutely crucial to retain credibility. Giving false reassurance is the worst thing one can do.
The first symptoms were sore throat, fever and headache. Then dizziness, loss of hearing, delirium, and convulsions. Some people turned brown. However, it wasn't the flu virus that killed most people. Rather, bacterial pneumonia was the killer. People could die within a day of commencing to cough.
The doctors tried various ineffective remedies, even encouraging smoking in the belief that smoke killed the microbes. They sought to combat a particular bacterium, thinking mistakenly that it was the cause of the flu, but It was just a secondary infection. It was not known that a virus was the real culprit, as viruses could not be detected in those days. The virus responsible was not identified till 1932. Only one therapeutic measure, transfusing blood from recovered patients to new victims, showed any hint of success.
Schools were closed but churches remained open. Masks were compulsory in the US, but they were useless. Except for a few localities, nearly all attempts to limit the spread failed. Treatment was also ineffective. The epidemic ended because the flu burnt itself out. Survivors were immune.
The 1918 pandemic did not infect everyone on the planet, nor even the 60% needed for herd immunity. It is estimated that it infected "only" 25% of the world population. So why did it go away? My reading states that people either died or were immune, causing the virus to die out. However, this begs the question of what about the 75% of the population who were not infected?
One theory holds that the 1918 virus mutated extremely rapidly to a less lethal strain. This is a common occurrence with influenza viruses: there is a tendency for pathogenic viruses to become less lethal with time, as the hosts of more dangerous strains tend to die out. Yet this would not explain why people were no longer getting infected. Perhaps a clue is that the three waves of the pandemic lasted 2-3 months each, as shown in the graphic. So maybe changing weather had something to do with it. They probably did not bother to add the small number of deaths in the southern hemisphere to the graph of 3 waves.
There is the further question of why each of the three waves ended before infecting 60%. A strange feature of the Spanish flu is that after the lethal second wave struck in late 1918, new cases dropped abruptly - almost to nothing after the peak in the second wave. This may have been due to changes in the virus itself. One can understand the logic of the virus mutating to less lethal forms, but surely it is also likely to mutate to more, rather than less, contagious forms? That would cause more infections even if causing fewer deaths. Yet this did not seem to happen.
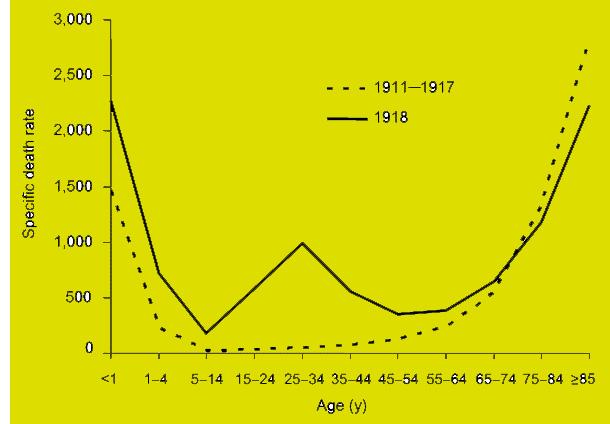
Most influenza outbreaks disproportionately kill the very young and the very old, with a higher survival rate for those in between, but the Spanish flu pandemic resulted in a death-rate spike at age 30, as well as with the very young and very old. Scientists offer several possible explanations for the high young adult mortality rate of the 1918 pandemic. Some analyses have shown the virus to be particularly deadly because it triggers a cytokine storm (overreaction of the body's immune system), which ravages the stronger immune system of young adults. In contrast, a 2007 analysis of medical journals from the period of the pandemic found that the viral infection was no more aggressive than previous influenza strains. Instead, malnourishment, overcrowded medical camps and hospitals, and poor hygiene promoted bacterial infection, which killed most of the victims.
The Spanish flu was the first of two pandemics caused by the H1N1 influenza virus, with the second being the swine flu in 2009.
Globally, the World Health Organization estimates that seasonal flu kills between 290,000 and 650,000 people per year. The flu kills about 3,500 people in Australia each year.
Epilogue
The parallels between 1918 and 2020 should not be stretched too far. The 1918 pandemic was a flu, unlike the corona virus called SARS CoV2, which is a respiratory disease causing the pandemic in 2020. The virus that causes Covid-19 is from the same family as the common cold and the SARS outbreak of 2003.